Complementary therapy in renal care
“Complementary therapies are therapies that run alongside conventional medicine. We as complementary therapists never diagnose or advise patients about medication. Instead, we help the patient with all the symptoms that come with kidney failure and dialysis.
“For example, many patients struggle with bone and muscle pains, headaches, nausea, irritable legs, and a numbing sensation in their feet and hands and fingers. Some of the older dialysis machines can also cause muscle spasms. We teach patients massage techniques and offer them various aromatherapy blends to help them relax. We also use essential oils to help manage symptoms. We have own blends of oils; our blue blend contains analgesic (painkiller) oils which are good for bone pain, muscle spasms, and headaches. Eucalyptus is beneficial for the colder months, and Bergamot and Chamomile are good for itchiness, for patients who feel like they want to scratch their skin off.
“Foot and leg exercises can offer relief, too. There are lots of different practical ways to help keep the flow of blood circulation during dialysis and this can help with numbness and pins and needles.
“Complementary therapy is about improving and enhancing the quality of life for patients, not just physically but also psychologically.
“For example, patients might be anxious if they find it painful being put on and off dialysis so we can help them relax through breathing techniques and meditation. Stress can be a major issue too, so we often work on that.
“Patients can struggle with attending dialysis three times a week, and a lot of patients don’t work and have financial concerns. Often, patients just want someone to talk to. Dialysis nurses are so dedicated and busy, so that’s where we as complementary therapists come in. Having a little chat to the patients can make all the difference. They look forward to us going in and we build relationships with them and their families.
“Dialysis patients will often have other medical conditions and complementary therapy is not just about kidney failure, it’s about looking at the bigger picture. We think about the whole patient, discussing what treatment they would like and adapting to each patient’s need, always checking with the clinicians in charge. We don’t want to overstimulate or under stimulate, so we tend to keep our therapies to a short 20-minute treatment.”
“The response we get is amazing; it’s all worthwhile when we go into the units and see the patients”
“I love to share knowledge, I support and co-ordinate FHT (Federation of Holistic Therapists) meetings locally. There are lots of people who need help and support through their medical journey and chronic kidney disease (CKD) is a massive thing. I started my journey and became passionate about alternative therapies in my early 20s. I completed diplomas in various therapies, a foundation degree at Wigan & Leigh College, and then a BSc (Hons) in Complementary Therapies (Integrated Therapies in Practice) at Salford University. There was a great amount of research involved. We also studied modules including mindfulness and breathing techniques. During my foundation degree, we had to complete 150 hours in a work setting. I chose a clinical setting and was introduced to the Wigan Renal Dialysis Unit. That was my passion, and the first day when I went onto the dialysis unit I thought: ‘This is me. This is what I want to do’. I became a volunteer myself and attended Wigan Dialysis unit for over three years before applying for my job. I later went on to study a PGDE teaching qualification at Bolton University so that I could teach Therapies.
“During the time I was volunteering, my consultant approached me and said the hospital wanted to get funding for a complementary therapist paid role. I applied for the job (publicly) and then Kidney Care UK provided the funding for my part-time employment for the first five years. The role then became permanent, and I was taken on by the Salford renal department.”
“We always keep our complementary therapy training and knowledge up to date, as things change so rapidly. I run training for the volunteers before they come onboard at the hospital, updating them about kidney failure and what that can mean. I’m also the Federation of Holistic Therapists (FHT) coordinator for the North of England and I help other therapists in our area. The units we cover under Salford, which is the main one, are Wigan, Bolton, Oldham, and Rochdale.
“It can be daunting for trainees, and as complementary therapists we do years and years of studying to understand how therapies work with medication and the body. All our volunteer therapists must have a Level 3 Diploma and must be a member of FHT or another professional body in order to work with dialysis patients.
“The therapy team are absolutely amazing. They give their time for free, coming on the units and offering whatever help they can. The response we get is amazing; it’s all worthwhile when we go into the units and see the patients. They so look forward to our team going in.
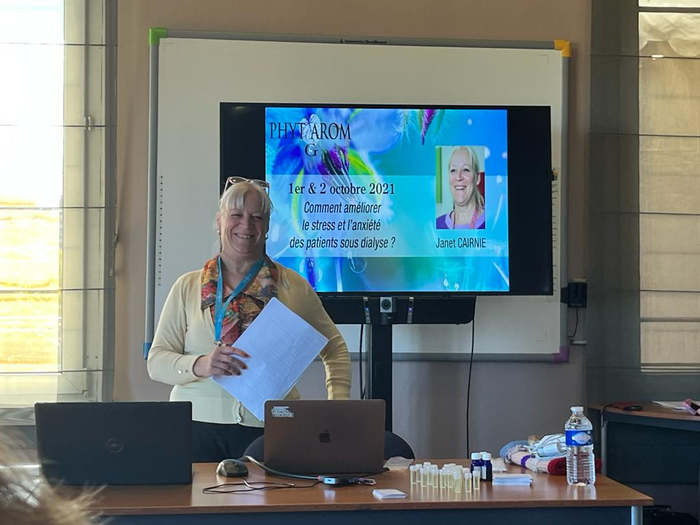
“The team has won various awards, including the Complementary Therapy Award for the Pain Management category and an FHT Excellence “Volunteer Service Award”. At the awards ceremony I made the point that complementary therapy should be available to all dialysis patients. It’s rare to see complementary therapists working with CKD patients. I went to France recently and no-one in Europe knew about complementary therapy on dialysis units. Therapy should be open to every patient, and I’m looking forward to the future. We’re needed now, more than ever.”

Complementary therapy: what people living with kidney disease need to know
“First and foremost, consult your doctor or a health professional before trying any form of complementary therapy.
“At Salford, we walk around units and make ourselves known to patients. There is a form that patients need to fill in where they can request different therapies and consent to therapy. We do everything we can to keep our patients safe.
“The FHT has a register if you want to find a therapist near you (you can filter by particular areas of expertise). You can also ask a member of your kidney team for information about complementary therapy in your unit or area, or feel free to get in touch with me via my email for advice. There are lots of different leaflets and information I can send about different therapies.”
“You should be mindful of the effects that complementary therapy can have:
- Some herbs and oils interact with medication (for example, citrus essential oils, including lemon, lime, orange, and bergamot, are known to cause photosensitive reactions). .
- Some immune boosting herbs should not be taken with certain medication.
- Some supplements can interact with blood thinners.
- Mood enhancers can have an effect on blood pressure.
- Over the counter sleep aids shouldn’t be mixed with alcohol, can affect blood pressure, and can have negative sedative effects.
“Complementary therapies should never be used in place of conventional medical care or medication. Always consult your doctor for medical care and diagnosis. Always advise your doctor or other healthcare professional if you are receiving complementary therapy healthcare.”
