Chronic kidney disease (CKD) means that your kidneys do not work as well as they should. Chronic means that it is a long-term condition that will last for the rest of your life.
Kidney failure is a severe form of CKD where your kidneys can no longer work well enough to keep you healthy. Kidney failure is also sometimes called end stage kidney disease (ESKD).
This leaflet gives more information about both CKD and kidney failure, as well as their causes, symptoms and treatments.
CKD and kidney failure can affect people in different ways. It is important to talk to your healthcare team about your specific situation and requirements.
What is chronic kidney disease (CKD)?
Chronic kidney disease (CKD) is a long-term condition where your kidneys do not work as well as they should.
CKD is very common. It affects around one in 10 people in the UK.
It can affect people of all ages but older adults aged over 60 are more likely to develop CKD.
CKD can run in families and is more common in people from Asian and Black backgrounds.
Some people are at increased risk of developing CKD because they have other conditions such as diabetes, high blood pressure or heart disease.
Only one in 50 people with CKD will develop kidney failure.
What causes CKD?
There are lots of causes of CKD including:
- diabetes
- heart disease
- high blood pressure (hypertension)
- inflammation within the kidneys (glomerulonephritis)
- long-term, regular use of certain medicines including non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen
- inherited kidney conditions that run in families
- rare diseases which account for one in 10 cases of CKD in adults and almost all cases in children.
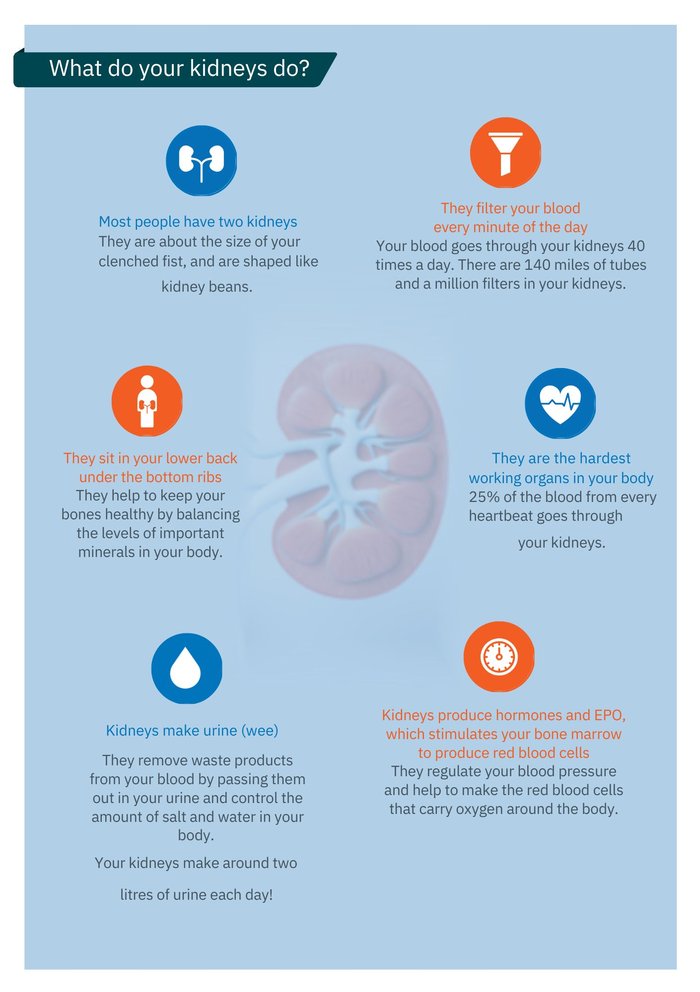
What happens to the body during CKD?
Your kidneys play a vital role in keeping your body healthy. If you develop CKD:
- waste products and excess fluid start to build up in your body as your kidneys can’t remove them properly
- your kidneys produce fewer red blood cells which can lead to anaemia
- damage to your kidneys’ filter system lets blood and protein leak into your urine
- your bones become weaker as your kidneys can no longer keep them strong and healthy.
What are the symptoms of CKD?
Most people do not have symptoms in the early stages of CKD. Even damaged kidneys can still work well enough to prevent any noticeable problems. However, kidney damage can still affect your health. CKD can increase the chance of developing high blood pressure, heart disease or a stroke. Early diagnosis and regular monitoring are therefore very important as lifestyle changes and medical treatment can help to slow the progression of CKD.

How is CKD treated?
There is currently no cure for CKD. In the early stages of CKD, treatment aims to help control the decline in your kidney function and manage any symptoms. This can include:
- Controlling your blood pressure. High blood pressure can speed up kidney damage. You may be prescribed blood pressure medication to keep your blood pressure under control. This is often in the form of medication such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs).
- Stabilising your kidney function. Sodium glucose co-transporter-2 (SGLT2) inhibitors slow down the progression of your kidney disease and lower the risk of developing heart failure.
- Preventing bone damage. Vitamin D supplements may be prescribed to help keep your bones healthy and strong.
How is CKD diagnosed?
CKD is usually diagnosed by blood and urine tests. You may have these tests as part of a normal check up with your doctor, or because your doctor thinks you may have CKD.
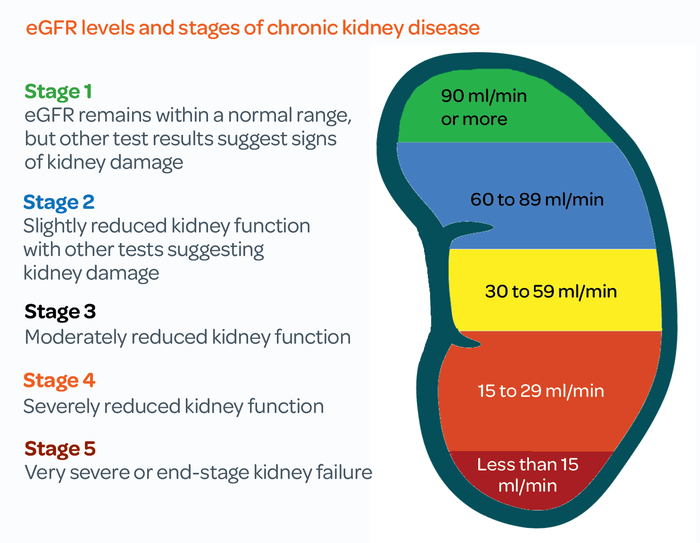
There are five stages of CKD. It starts at stage 1 and can go up to stage 5 if it gets worse. The stages are based on a measurement called the glomerular filtration rate (GFR). Glomeruli are the network of tiny blood vessels inside the kidneys that separate out waste products and excess fluid from the blood. GFR shows how well the kidneys filter the blood, by indicating how much blood passes through the glomeruli every minute.
Getting an accurate measurement of GFR is difficult, so blood test results normally give an estimated filtration rate (eGFR). eGFR may be listed as a measurement of ml/min or as a percentage. So, an eGFR of 50ml/min means your kidneys are functioning at about 50%.
In some cases, kidney function can drop suddenly and then improve. This is known as acute kidney injury (AKI) and normally happens as a complication of another condition. AKI is usually temporary. This is different from CKD which does not get better, but can be slowed or managed with treatment.
- Most people with CKD stages 1, 2 and 3 manage the condition themselves with support from their GP. This could be things like taking medicine and eating a healthy diet.
- If your CKD reaches stage 4, your doctor will send you to a specialist kidney doctor, called a nephrologist, at a hospital to discuss further treatment.
- If your CKD reaches stage 5, you will be classed as being in kidney failure. This is when your kidneys no longer work well enough to keep you healthy and specialist treatment is needed.
One in 50 people with CKD develop kidney failure.
What happens if I am diagnosed with kidney failure?
If you develop kidney failure, you will have regular appointments with your kidney team in the hospital to monitor your kidney function, treat any symptoms and discuss possible treatments.
This may be as part of an advanced kidney care or low clearance clinic.
What are the symptoms of kidney failure?
Common symptoms include:
- tiredness, low energy levels
- difficulty concentrating
- poor appetite
- changes in how things taste
- swollen ankles, feet or hands
- puffiness around the face, especially in the morning
- shortness of breath
- an increased need to wee, especially at night
- difficulty sleeping
- itchy skin
- muscle cramps or weakness
- feeling sick
- headaches

How is kidney failure treated?
Although there is currently no cure for kidney failure, the three main treatments are: a kidney transplant, dialysis or conservative kidney management (also known as conservative or supportive care).
A transplant is an operation to place a healthy kidney from someone else (a donor) into a person with kidney failure.
The new kidney can come from someone who has died (deceased donation) or from a living donor (living donation). This may be a friend or relative. Talk to your kidney team about this.
There are about 7,500 people waiting for a kidney transplant in the UK at the moment. The average waiting time for a deceased donor kidney is around two to three years.
You need to be reasonably healthy to have the operation and for your body to cope with the medications you will need to take to prevent rejection of the new kidney. Your kidney team will let you know if transplant is a suitable option for you.
A successful transplant is a very good treatment for kidney failure. However, it will not cure the underlying cause of your kidney disease. Some kidney diseases can reoccur in the transplanted kidney.
On average, a kidney transplant from a living donor will last for 20-25 years, while a kidney from a deceased donor will last 15-20 years.
Around one in every 10 patients have rejection in the first year after a transplant. Rejection means that your body's immune system is attacking your transplanted kidney. This might mean that you need to go on dialysis or have another transplant in the future. Your kidney doctor will discuss this with you.
Dialysis is a treatment that uses a machine or device to clean your blood. This is what kidneys do on their own if they are healthy. Dialysis is a treatment for kidney failure but it will not cure it. Once you start dialysis you will need to continue with it for the rest of your life, or until you receive a kidney transplant.
If you are having dialysis, you may be advised to make changes to your diet or limit how much fluid you drink. Your healthcare team will give you individual advice and may refer you to a specialist kidney dietitian.
There are two main types of dialysis:
Haemodialysis (HD) cleans your blood by putting it through a dialysis machine. The clean blood is then returned to your body and the dialysis fluid that helps to clean your blood is thrown away.
Most people have haemodialysis three times a week, with each session lasting around four hours. You can have haemodialysis in hospital or in a separate specialist dialysis unit. You may also be able to do your own dialysis at home (home haemodialysis).
Peritoneal dialysis (PD) uses the inside lining of your abdomen (the peritoneum) to clean your blood, inside your body. A special fluid called dialysate is sent from a bag into your abdomen through a catheter. Dialysate is made up of water, salts and other additives. The dialysate absorbs waste, extra salts and water from your body. It is then drained out of your body, taking the waste, extra salts and water with it.
Peritoneal dialysis is done at home, and most people have PD every day. Your kidney team will show you how to perform the treatment yourself.
There are two main ways of doing your peritoneal dialysis.
Continuous ambulatory peritoneal dialysis (CAPD) is where you do your treatment in the day time. Each treatment or exchange takes about 30 to 40 minutes. You will normally have between one and four exchanges each day.
Automated peritoneal dialysis (APD) is where a machine does your exchanges overnight while you sleep.
Conservative or supportive care, also known as conservative management, focuses on managing the symptoms of kidney disease and keeping your kidneys working for as long as possible without dialysis or a transplant.
This includes:
- regular appointments with your kidney team
- controlling your blood pressure to protect your kidney function
- treating any symptoms of kidney failure like itching and anaemia
- advising you on changing your diet to help you feel better
- helping to make plans for your future
Kidney failure: deciding which treatment is best for you
Lots of factors might affect your treatment decisions, including the cause of your kidney disease, your lifestyle, work and family life.
Your kidney team can provide specialist advice to help you understand your treatment options.
| Transplant | Haemodialysis (HD) | Peritoneal dialysis (PD) | Conservative or supportive care | |
|---|---|---|---|---|
Will it replace my kidney function? |
Yes |
Yes |
Yes |
No |
Where does the treatment take place? |
In hospital |
In hospital, clinic or at home |
At home |
At home |
How often will I need treatment? |
Surgery and ongoing medication; more than one transplant may be needed |
Usually 3 days a week |
3-4 times a day or overnight |
No set times for treatment |
How long does each treatment take? |
You may have to wait several years for a suitable transplant |
Usually 4 hours |
30-40 minutes for each daytime session or 8-10 hours overnight |
No set times for treatment |
Will I need any equipment at home? |
No |
Yes if you have dialysis at home |
Yes |
No |
How long can I live with kidney failure?
Kidney failure is a serious condition that can affect your life expectancy.
The younger and healthier you are when you are first diagnosed with kidney failure, the longer your life expectancy is likely to be.
Transplant is often the best treatment for improving life expectancy, but it is not a suitable option for everyone.
Dialysis usually increases life expectancy, but this is not always the case for older patients and those with other health problems.
Overall, people choosing conservative or supportive care tend to live for a shorter length of time than those choosing dialysis or transplant, because conservative care does not improve kidney function.
It is important that you discuss your treatment options and preferences with your kidney team, as well as your family and friends. Treatment for kidney failure is an individual choice.

What support is available for me?
Finding out that you have kidney failure can have a big impact on your life. You may feel overwhelmed by all the information you are given, especially if the diagnosis was unexpected. It is important to take time to think about what you have been told.
- Make a list of things you want to discuss with your kidney team before your appointment
- Ask for written information that you can read in your own time
- Take notes in your appointments, so you remember what your kidney team tell you
- Ask for access to your blood and urine test results
- Ask to see a kidney social worker for advice on benefits or a counsellor to talk to about your emotional health.
- Talk to your manager or Human Resources department
- Discuss whether there are any changes that might help you, such as flexible hours to fit in with your treatment
- For more information see our leaflet on Employment rights.
Ask a family member or friend to come with you to appointments. They can help you remember what was said and may ask questions that you have not thought about.
Ask your kidney team if there is a local kidney patient support group. Many people find it very helpful to connect with other patients and carers.
Work with your kidney team to agree on a care plan. This lists your personal choices and treatment preferences. Making these plans in advance and when you are still feeling well can help ensure that your wishes are carried out at a future time when you may be too unwell to express them.
Find out more about Kidney Care UK's free patient support services.

Publication date: 06/2025
Review date: 06/2028