Please note: the following information is for employers of kidney patients. If you are a kidney patient, see our page on employment rights for people living with CKD.
This page gives more information about CKD and its treatment, how this may affect your employee and what you can do to help.
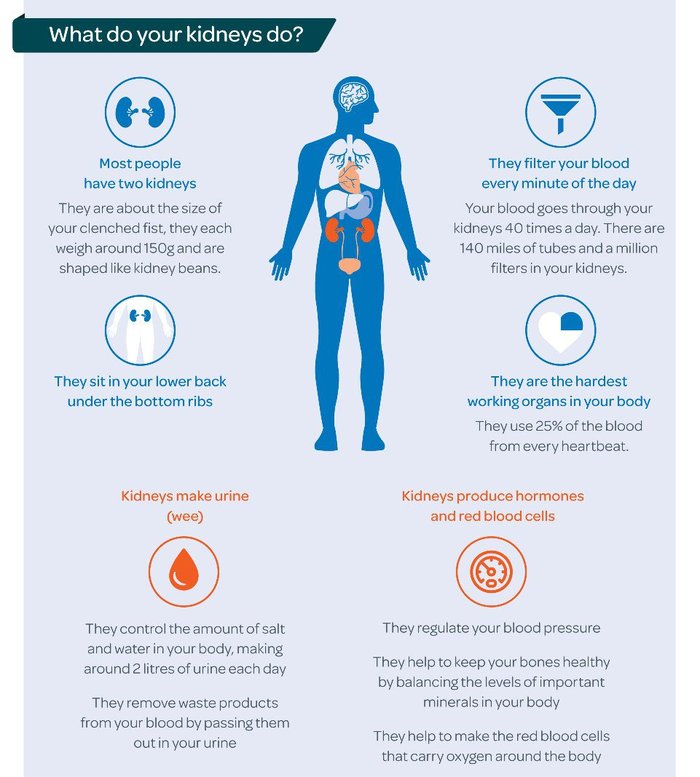
Chronic kidney disease (CKD) is a long-term condition where the kidneys do not work as well as they should. They may have been damaged or affected by disease.
CKD can affect people in different ways. It is therefore important to talk to your employee in confidence about their specific situation and requirements.
What is CKD?
If you have CKD, your kidneys do not work as well as they should. Waste products start to build up in your body as your kidneys can’t remove them properly. Damage to your kidneys’ filter system lets blood and protein leak into your urine.

How is CKD diagnosed?
CKD is usually diagnosed by blood and urine tests.
CKD is divided into five stages based on the glomerular filtration rate (GFR). Glomeruli are the network of tiny blood vessels inside the kidneys that separate out waste products and excess fluid from the blood. GFR shows how well the kidneys filter the blood, by indicating how much blood passes through the glomeruli every minute.
Getting an accurate measurement of GFR is difficult, so blood test results normally give an estimated filtration rate, or eGFR. eGFR may be listed as a measurement of ml/min or as a percentage. So, an eGFR of 50ml/min means the kidneys are functioning at about 50%.
Most people with CKD stages one to three manage the condition themselves with support from their GP and do not need any specialist care from kidney doctors.
If CKD progresses to stage four, a referral to a hospital-based kidney doctor (nephrologist) is needed for further treatment. CKD can get worse over time, although in the majority of people it will not progress to stage four.
Only one in 50 people with CKD will need dialysis or a transplant.
Is it common?
CKD is very common. It affects around one in ten people in the UK. The vast majority of people with CKD do not have any symptoms.
Who gets CKD?
CKD can affect people of all ages, including babies and children. It can run in families and is more common in people from Asian and Black backgrounds.
Some people are at increased risk of developing CKD because they have other conditions such as diabetes, high blood pressure or heart disease.
| Stages of Chronic Kidney Disease | Description | eGFR levels |
|---|---|---|
| 1 | eGFR remains within a normal range, but other test results suggest signs of kidney damage | 90 ml/min or more |
| 2 | Slightly reduced kidney function with other tests suggesting kidney damage | 60-89 ml/min |
| 3 | Moderately reduced kidney function | 30-59 ml/min |
| 4 | Severely reduced kidney function | 15-29 ml/min |
| 5 | Very severe or end-stage kidney failure | Less than 15 ml |
What causes CKD?
There are lots of causes of CKD including:
- Diabetes
- Heart disease
- High blood pressure (hypertension)
- Inflammation within the kidneys (glomerulonephritis)
- Long-term, regular use of certain medicines including non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and naproxen
- Family history including inherited kidney conditions and rare diseases which account for one in ten cases of CKD in adults and almost all cases in children.
What are the symptoms of CKD?
Early stage CKD (one to three)
Most people do not have symptoms in the early stages of CKD, as even damaged kidneys can still work well enough to prevent any noticeable symptoms.
Late stages of CKD (four to five)
Symptoms include:
- weight loss and poor appetite
- swollen ankles, feet or hands
- puffiness around the face, especially in the morning
- shortness of breath
- tiredness, low energy levels
- blood in your urine
- an increased need to wee, especially at night
- difficulty sleeping
- itchy skin
- muscle cramps or weakness
- feeling sick
- headaches
Although many people do not have any symptoms, kidney damage can still affect their health. CKD can increase the chance of developing acute kidney injury, high blood pressure, heart disease or a stroke. Early diagnosis and regular monitoring are therefore very important as lifestyle changes and medical treatment can prevent CKD from getting worse.

How is CKD treated in stages one to three?
People with mild CKD (stages one to three) and stable kidney function are unlikely to need any specific treatment and will be monitored by their GP. They may receive treatment for some of the symptoms of kidney disease, including anaemia, and treatment to keep the bones healthy.
How is CKD treated in stages four to five?
More severe CKD (stages four to five) is likely to need specialist treatment such as dialysis, a kidney transplant or conservative kidney care. All treatments are provided free of charge by the NHS.
Dialysis
Dialysis is a treatment that removes the toxins and excess fluid from the body that the damaged kidneys cannot get rid of.
There are two main types of dialysis:
Haemodialysis (HD) ‘cleans’ the blood by running it through a dialysis machine filter. The clean blood is then returned to the body and the dialysis fluid is thrown away.
Most people have haemodialysis three times a week, with each session lasting around four hours. It usually takes place in hospital but some people train to do their own dialysis at home. If your employee is receiving dialysis in hospital, they will be given a specific time slot to attend hospital and it is very important that they go to every appointment.
Peritoneal dialysis (PD) uses the inside lining of the abdomen (the peritoneum) to filter the blood, within the body. This filtering removes waste products that have built up in the blood stream. A special fluid called dialysate, which contains water, salts and other additives, flows from a bag into the abdomen through a soft tube called a catheter. The catheter stays in the abdomen all the time, with part of the catheter on the outside of the body.
Your employee can perform PD themselves. Each treatment takes about 30 to 40 minutes, and four to six treatments are usually needed each day. Alternatively, they may choose to have automated peritoneal dialysis (APD), which is done by a machine overnight while they sleep.
Dialysis is a treatment but not a cure for CKD. Once your employee starts dialysis they will need to continue with it for the rest of their life, or until they receive a kidney transplant.
Kidney transplant
A transplant is an operation to replace the damaged kidneys with a new kidney from either a living or deceased donor.
There are about 6,000 people waiting for a kidney transplant in the UK at the moment and the average waiting time for a kidney is around two to three years.
Your employee may be called for a transplant at very short notice and will need time off work to recover afterwards. This will usually be around two to three months but may be shorter depending on their job and your employee’s health. A phased return to work is likely to be helpful and you should discuss this with your employee and your Human Resources (HR) department.
On average, a kidney transplant from a living donor will last for 20 to 25 years, while a kidney from a deceased donor will last 15 to 20 years.
A transplant should improve your employee’s health and quality of life, and prevent the need for dialysis, but it is not a cure. Most transplant recipients will still have some form of kidney disease and will need to take medicines for the rest of their life and attend regular check-ups.
There is a small chance that the new kidney will not work or is later rejected. This might mean that your employee needs to go back on dialysis or requires another transplant in the future.

Conservative kidney management
Conservative care focuses on managing the symptoms of kidney disease and maintaining quality of life without going on dialysis or having a transplant.
Conservative kidney management includes:
- Regular appointments with the kidney team
- Monitoring and controlling blood pressure to protect kidney function
- Treating any symptoms of kidney failure like itching
- Helping to make plans for the future
Dialysis helps to keep people with kidney failure alive until they receive a transplant, so choosing conservative kidney management is life-limiting.
More information on treatments.
It is very important that everyone with CKD attends their appointments at their GP surgery or hospital to have their kidney function checked and any treatment monitored.
I have been working for our supermarket’s Head Office for 33 years. They have supported me through two of my three kidney transplants and 15 of my 22 years on dialysis. They gave me a private room with a key to do my dialysis at work and they let me do flexitime around my many appointments. They have been brilliant.Paul, kidney patient
What can I do to help?
Employees with health conditions, including chronic illnesses, are afforded protections under employment law. Many people with kidney disease will meet the definition of disability under the Equality Act 2010.
Employers are required to make reasonable adjustments to support employees with disabilities and must not discriminate on the grounds of disability.
Encourage your employee to talk to you and your HR department to discuss how reasonable adjustments can be made to make their working life easier. This will depend on their individual work situation but could include:
- Conducting a workplace assessment. See the ACAS website for advice
- Changing their hours to suit their dialysis schedule
- Allowing them time off work to attend their hospital appointments
- Changing their job responsibilities – for example, to avoid heavy lifting if they are on dialysis or have had a transplant
- Allowing them to work from home for some or all of the week
- Providing access to an occupational therapist
- Allowing your employee access to a private space such as a first aid room if they need to carry out PD during work hours
- Providing adapted computer equipment or better seating
- Allowing them to take more breaks if they need them
- Keeping in touch with your employee if they are off sick, without pressuring them to return to work before they are ready.
I work as a bus driver and have always been upfront about my kidney issues. With the support and encouragement of my employers, I have achieved 100% attendance at work in three out of the four years that I have been on dialysis. Going on dialysis was a very stressful time for me but being able to take away the worry of the impact it would have on my job has made the process so much more bearable.Tony, kidney patient
Where can I find out more information?
- Kidney Care UK - Get support
- Advisory, Conciliation and Arbitration Service (ACAS) - Disability at work
- Citizens Advice - Work
- NHS - Chronic kidney disease

Publication date: 10/2024
Review date: 10/2027