People with chronic kidney disease (CKD) need to take special care of their feet because kidney disease can damage the nerves and blood vessels. This can increase your risk of having heart attack or stroke. CKD can affect:
- the blood circulation in your feet (ischaemia)
- the feeling in your feet (peripheral neuropathy).
These changes can be very gradual and so may be hard to notice. They are more common in people with advanced CKD (stages 4 and 5), especially if they also have diabetes or other health conditions.
It is recommended that people with CKD have their feet checked regularly by a healthcare professional. Talk to your GP if you have any concerns or visit a podiatrist (an expert in foot care).
What foot problems can occur in people with CKD?
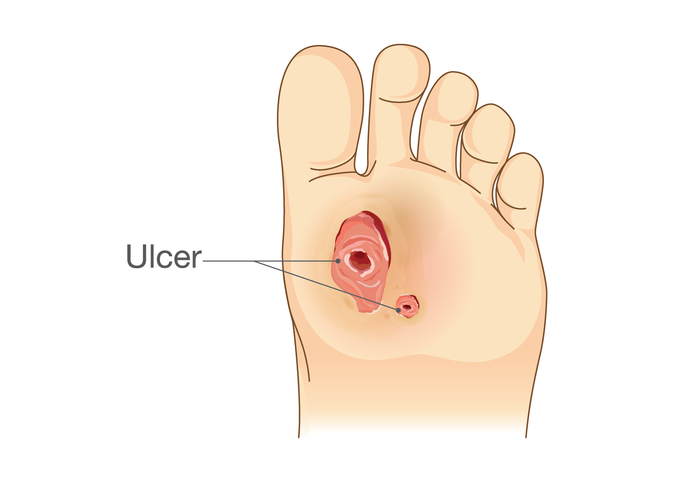
Foot ulcers
An ulcer is an area of skin that has broken down so that the tissue underneath is exposed. Ulcers are more common in people with CKD as the skin does not heal very well after a cut. Ulcers can become infected if they are not treated properly. An infection can cause serious complications including sepsis (a life-threatening reaction to an infection) and an increased risk of amputations of the foot or leg.
Foot ulcers need specialist review and treatment by a podiatrist. You may also be referred to other healthcare departments for treatment. Do not try to treat an ulcer on your own as you may make it worse. Foot ulcers are sometimes hidden beneath a layer of hard skin, known as a callus. Your podiatrist may need to reduce or remove the callus or any blistered skin to help the ulcer to heal.
You may be offered a cast or special shoe to wear to reduce the pressure on the ulcer until it has healed.
You may also be prescribed antibiotics if there are signs of infection. Severe infections may need an operation to clean the ulcer and infected tissue. In very severe and rare cases, an amputation may be needed to reduce the risk of further infection.
Charcot foot
Charcot foot is a very serious complication that is linked to nerve damage in your feet. Although it does not usually cause any pain, it can make the bones of your feet very fragile so they may break or dislocate easily, even after minor injuries. You are at a greater risk of this if you also have a diagnosis of diabetes.
Charcot foot can lead to serious complications, including an increased risk of ulcers and amputations of the foot or leg.
Your foot may permanently change shape if you do not get appropriate treatment early enough and you continue to walk on it.
The early signs of Charcot foot are swelling and warmth in the affected area of the foot or ankle. There may also be some redness or change in colour. In most cases only one foot is affected. In rare cases people can develop Charcot foot in both feet, although not at the same time.
Treatment aims to prevent a permanent change to the shape of your foot. This is done by reducing the pressure on your foot by using either a non-removable plaster cast (in the same way as if you had broken a bone), or a removable walker boot. After the Charcot foot has recovered, you may need an offloading shoe or prescription insole to prevent further problems in the future.
How can I reduce the risk of foot problems?
You can reduce your risk of developing foot problems by:
- covering any cuts or blisters with a clean dressing or plaster. Do not burst blisters
- keeping your blood pressure and cholesterol levels under control
- stopping smoking
- maintaining a healthy weight and staying active
- managing other conditions that you may have, such as diabetes
- following any dietary and healthcare advice from your kidney team
- making sure you have properly fitting footwear, that is the correct size and both wide and deep enough for your foot shape.
Contact your podiatrist or medical team straight away if your foot is painful, hot or throbbing or if there is any discharge, swelling or discolouration to the skin.
How can I take care of my feet?
- Check your feet every day for any changes in colour, temperature or shape, or any signs of injury or breaks in the skin. Seek advice from a podiatrist or GP if you have any concerns.
- Wash your feet every day in warm water with a mild soap. Rinse them thoroughly and dry them carefully, especially between the toes. Do not soak your feet as this can damage your skin.
- If your skin is dry, apply a moisturising cream every day, to the top and bottom of your feet, avoiding the areas between your toes.

- Seek advice from a podiatrist or GP before you attempt to remove hard skin or corns (small lumps of hard skin on your feet) yourself. They will give you advice on how to best look after your feet or will treat any problems for you. Never use over-the-counter corn remedies as they contain acids which could damage the skin and might lead to an ulcer.
- Wear well-fitting shoes indoors and outdoors and avoid walking barefoot to reduce the risk of injury to your feet.
- Keep your toenails short and neat. If you feel confident or have someone who is able to help you, cut or file your toenails following the curve of the end of your toe. Use a nail file to make sure that there are no sharp edges which could press into the next toe. Do not cut down the sides of your nails as you may create a ‘spike’ of nail which could result in an ingrown toenail.
- Change your socks, stockings or tights every day. Avoid bulky seams or elasticated tops of socks as these can reduce the circulation in your legs or cause ridges and areas of increased pressure if they are too tight. Check that your socks, stockings or tights are not too tight around the ends of your toes.
- Wear an extra pair of socks if your feet are cold. To reduce the risk of burns, avoid sitting with your feet in front of the fire or radiator to warm them up. Remove hot water bottles or heating pads from your bed before getting in to prevent accidentally burning your skin. Check the temperature of your bathwater with your elbow before you get in, or ask someone else to do it for you, to make sure the water is not too hot.

- Keep your feet covered in the summer or use a high-factor sun-protection cream (SPF 30 or higher) to protect them from sunburn and ensure you apply it regularly throughout the day.
- Check the bottom of your shoes before putting them on to make sure that nothing sharp has pierced the sole. Feel inside each shoe to check for any small objects such as pebbles that may have fallen in.
- Check your shoes for signs of damage such as rough seams, worn soles or heels. Replace damaged shoes if they can’t be repaired.
- Your feet can change shape over time. Try to have them measured when you buy new shoes to make sure they fit correctly and do not press on your toes. Always try on both shoes as most people’s feet are slightly different sizes.
- Long journeys with prolonged periods of sitting can make your feet swell. Try to get up and move about every half an hour, even if it’s just for a short walk. This will keep your circulation going and reduce swelling.
- Attend all of your podiatry and other healthcare appointments
What type of shoes should I wear?
Shoes or boots with laces or strap fastenings will give your feet the best support and help to keep your foot firmly in place, which will help prevent rubbing. If the depth of your shoe is too shallow, this can lead to pressure on your feet. Make sure that the fastening keeps the middle of your foot and your heel in place and that you have enough room to wiggle your toes naturally.
Avoid slip-on shoes, flip-flops and slippers without any fastenings, as they give less support to your feet. Slippers with a velcro strap or zip are recommended.
The uppers (top) of your shoes or boots should be made from a natural material such as leather. This will help them fit to your feet without causing any rubbing and will also help prevent your feet from sweating.
Avoid seams or rigid stitching around the toes of your shoes to prevent any rubbing.
The heel of your footwear should not be more than 2.5 centimetres (1 inch) high.
You may be prescribed special shoes or insoles by your healthcare team. Always follow their advice on how to wear them.

How can my kidney healthcare team help?
If you are receiving dialysis treatment (haemodialysis or peritoneal dialysis), ask your dialysis team if they can check your feet at least once a week.
They can check for any signs of corns, calluses (patches of rough, thick skin) or changes in your foot shape, colour or temperature.
They may recommend that you wear special protective boots during your dialysis session to reduce the pressure on your feet from the chair.
They may refer you to specialist podiatry care if needed.
If you notice any of the following problems, ACT NOW
- Accident or injury to a toe or foot
- Change in colour or shape, or swelling to a toe or foot
- Temperature change about your foot or lower limb
- New or unexplained pain in your foot
- Oozing or odour from a wound on a toe or foot
- Wound or break in the skin to a toe or foot
It is important that you contact your foot care team, local podiatry department or GP for advice as soon as possible (within 24 hours).
If your foot shows signs of increasing temperature, swelling, discharge, pain, or change in colour or shape, please contact 111 who may advise you to attend your local accident and emergency department.
Any delay in getting advice or treatment can lead to serious problems.
ACT NOW message courtesy of IDEAL Diabetes.
Where can I find out more information?
- Royal College of Podiatry: Common foot problems
- Legs Matter: Information and support for leg and foot problems
- The Healthy Footwear Guide

Publication date: 06/2025
Review date: 06/2028