Why do I need a fistula?
When your kidney function is declining to a point where you need treatment to take over the job of your kidneys, your kidney team will talk to you about your options, including haemodialysis.
To have haemodialysis, you need a way of connecting the dialysis machine to your bloodstream. This is called vascular access.
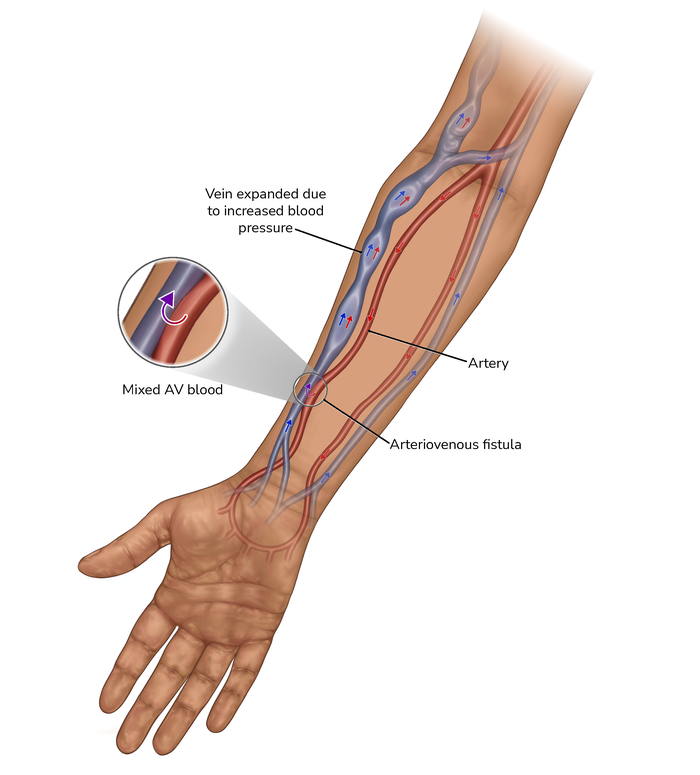
An arteriovenous (AV) fistula, usually just called a fistula, is one type of vascular access. It’s a blood vessel that’s created by joining together an artery and a vein in your arm. The result is a larger, stronger blood vessel, so lots of blood can flow through it smoothly.
When you’re having haemodialysis, the dialysis machine is connected to your bloodstream by tubes attached to needles, which are inserted into your fistula.
There are other types of vascular access, but a fistula is considered the gold standard. There’s evidence that patients who dialyse with a fistula have more effective dialysis, get fewer infections, and stay healthier for longer.
Your kidney team will help you decide which option is best for you.
What does having a fistula created involve?
An AV fistula is usually created in your non-dominant arm, and there are three positions or sites where the join is made. The vessel then develops up your arm. The three sites are:
- in your forearm close to your wrist (radio-cephalic)
- in or close to the bend of your arm in the centre (brachio-cephalic)
- in or close to the bend of your arm closer to your body (radio-basilic)
You need a minor operation to create the fistula. It’s a very safe procedure that can be performed under local, regional or general anaesthetic. If you have a brachio-basilic fistula made you may need additional surgery which requires a general anaesthetic and an overnight stay in hospital.
It involves making a small cut in your skin, deep enough so the vascular surgeon can access the vein and artery. The surgeon then cuts a tiny opening in the vein and one in the artery and reconnects them. This allows arterial blood to flow into the vein. The pressure this adds to the vein allows it to grow and develop so it can be used reliably for dialysis and act differently to all your other superficial veins.
You’ll have a short, thin scar – usually around 4cm to 6m in length – where your skin was opened up.
In the last few years, a new type of fistula has been developed called an endovascular arteriovenous fistula, or EndoAVF for short, which uses radiofrequency energy, rather than open surgery, to join the artery and the vein. EndoAVF is still in the development stage in the UK and is not offered in all units.
With both types of fistula, a clinician will either scan your arm or perform a clinical assessment to make sure it can be used for dialysis. A standard fistula usually takes around two to six weeks (sometimes longer) to be functional.
Official guidance recommends that you have a fistula created up to a year before your kidney team thinks you’ll need to start haemodialysis.
How will my everyday life be affected by a fistula?
Fistulas generally don’t require much in the way of maintenance; you can carry on with normal day-to-day activities.
When you have a tube permanently inserted into a blood vessel like you do with a dialysis line (central venous catheter) the tube must always be kept dry and away from water because of the risk of infection and dislodging the line.
One of the benefits of a fistula is that there is no direct access from the inside of the body to the outside when you are not on dialysis, allowing you to shower, bathe and swim without restriction.
When the needles are removed at the end of each dialysis session, it’s normal for the needling sites to bleed a little. Applying pressure with a piece of gauze or a cotton swab for a few minutes is normally enough to stop the bleeding.
Sometimes, a fistula can bleed spontaneously in between dialysis sessions. This should always be reported to your dialysis team, as it may be a sign that there is a problem with your fistula.
Applying direct pressure, as above, will usually stop the bleeding. In rare cases applying pressure isn’t enough to stop the bleeding, and it can quickly become serious. If this happens, it’s essential that you seek medical help urgently.
Why do fistulas make your arm look different?
A drawback of a fistula is that, over time, the blood vessels in your arm may become enlarged and bumpy because of high volumes of blood passing through, and needles being inserted into your fistula at every dialysis session.
This is completely normal and is a sign that your fistula is working well. But it can be very noticeable, and some people are uncomfortable or self-conscious about how their fistula looks.
If you’re worried about this and it’s affecting your body image, it might be worth talking to a member of your kidney team or a renal counsellor (Kidney Care UK offers a free renal counselling service to kidney patients and their families).
What’s the fistula “buzz”?
When a fistula is functioning well, the high volume of blood travelling quickly through it creates a ‘buzz’ or a ‘thrill’, which you can feel when you touch your arm where the fistula is located. You might find this strange to start with, but you’ll soon get used to it.
When you first start haemodialysis, using the fistula may be uncomfortable or painful. It can take time to adjust to having dialysis needles inserted into the fistula, but most people do so quickly.
If you have any questions or concerns about having a fistula, talk to someone in your kidney team.
5 things to discuss with your surgeon before a fistula operation
A fistula is one type of vascular access that enables you to have haemodialysis, and it is considered the gold standard for people who have dialysis. But it isn’t the only option. You should have the opportunity to discuss other types of vascular access like a graft or a tunnelled line, and other forms of treatment, like peritoneal dialysis and transplant.
It’s important to make sure you understand why your kidney team thinks having a fistula is right for you, so you can make an informed decision.
Dr Rajesh Sivaprakasam, consultant transplant and access surgeon at Barts Health NHS Trust, says: “It's my responsibility to justify to patients why I think they should have a fistula, rather than just telling them, ‘This is the treatment’. The patient is always involved in decision making.”
For most people, the answer is no. Having a transplant is the best form of treatment for people with chronic kidney disease, and generally people do better in the long term if they have a transplant before ever needing dialysis.
Everybody’s circumstances are different, though, and there may be a good reason for you to be put forward for dialysis, and so to have fistula surgery, before or instead of going on the transplant list.
The likelihood is you’ll have a standard arteriovenous (AV) fistula, which is created by connecting the artery and vein in your arm during a minor operation.
A new, less invasive type of fistula that doesn’t require surgery, called an EndoAV fistula, is an option for some people. Currently only a few centres offer the procedure, and you have to meet certain criteria to be suitable. But it’s worth asking your kidney team for more information.
Dr Sivaprakasam says: “This is something that needs to be spread across all units. We should champion patients and tell them there is this option. The limitation for these techniques is that they are suitable for 30-35% of patients. Maybe in the future we will be able to offer it to more people, but there is no guarantee.”
You can normally see your fistula under your skin and feel a buzzing sensation called a ‘thrill’. This is completely normal – it’s caused by lots of blood flowing through quickly – and is a sign that your fistula is working well.
Over time, fistulas get bigger and can appear quite twisty and lumpy, and some people are self-conscious about it.
Several factors could affect it, like the size and shape of your blood vessels, and where in your arm you have it created. Dr Sivaprakasam says: “Unfortunately, patients are often not given much time to discuss the fact that the scar and the appearance of their fistula will change, and what the effect on their life will be.”
It’s hard to imagine exactly what your fistula will look and feel like before you have the surgery. Your kidney team may be able to show you pictures or connect you with another patient who has a fistula, to give you some idea of what to expect, but every fistula is unique to the person and their arm. Your fistula will also continue to develop over time.
Around six to eight weeks after having your fistula creation surgery, you should have an ultrasound scan of your fistula to check it’s ‘mature’. That means it’s working well and is ready to be used for dialysis.
There’s no guarantee you’ll get a well-functioning fistula at the first attempt, and it’s important to talk to your surgeon and your kidney team about what options you might have if your fistula doesn’t take for any reason.
Problems can occur further down the line when you’ve been having dialysis for a while, too, like blood clots and aneurysms. They can often be resolved quite easily.